Robotics is a well-established usage in surgical practice. They have had their roles typified in neurology, endoscopic and more recently in the 5 to 6years gap in orthopaedics. One of the important healthcare challenges are in always improving the patient’s care, patient experience of care and translating that to population and reducing per capital cost in such improvements. WHO data shows there is a number of patient presenting with osteoarthritis. In Singapore, as well as many parts of the world there will be expected of increasing number elderly patients. Thus, people are working longer there is an important drive to optimising treatment for joint pain in younger patients and in older patients. The aim of any joint replacement especially in the lower limb (hip and knees) is to obtain optimal alignment, early return to work and have a long-lasting implant. In Singapore patients are working for an extended period of time thus, providing lower limb functionality is very crucial in enabling patients to carry on working in the extended period of the lifetime.
Robotics in arthroplasty has have a very established ground work in the last 5years. It involves clinical evaluation of patients as well as CT planning utilising specific protocols. This facilitates the surgeon in sizing the knee and also pre-operatively to plan any difficulties to be anticipated during surgery. This is very useful since prior to the surgery planning has been made to anticipate the potiential technical challenges, sizing and optimising kinematic placement of the components. This helps in reducing overall surgical time. In robotics patient often have a fear that the surgeon does not perform the surgery and it is done by the robot. However, contrary to the believe it is entirely surgeon operating on the procedure. When Dr Sathappan does Makoplasty which is a form of robotic assisted joint replacement the usage of computed aided technology allows controlled cuts and placement of components in optimal position. Safety zones are determine by what is term by haptic zone. This ensures that safety is not breached and the implants are put in optimal positions as determined by CT scan based data which is available pre-operatively.
Clinical studies by numerous authors has shown that Mako robotic assisted partial knee replacement has resulted in lower post-operative pain and very accurate implant placement in comparison to conventional partial replacement arthroplasty. Moreover, the patient satisfaction in such patients in the intermediate to mid-term has shown is in excess of 90%. Due to minimally invasive techniques (keyhole) patients require less physiotherapy and achieve the same functional goals of total knee replacement patients at a much shorter and faster time period. In the recent years the Mako robotic arm has been established in the usage of total hip replacement as well as total knee replacement. The suitability in utilising the robotic technology will be assessed in terms of the patient’s clinical presentation as well as the pre-operative CT scan.

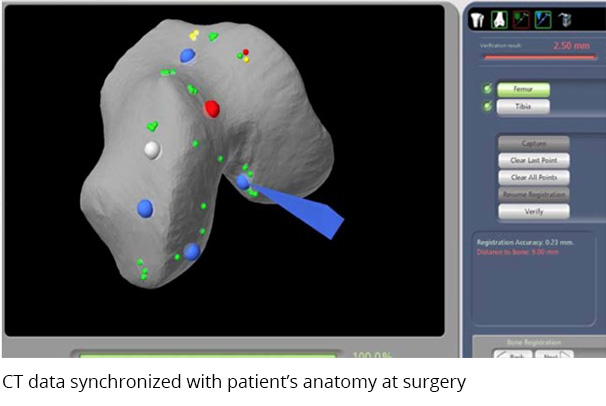
The procedure of Makoplasty first involves CT scan data acquisition and following this the images are clinically reviewed by the surgeon and appropriate analysis is facilitated for surgical planning. Registration is done during surgery. This involves synchronising the computer (Mako with the CT scan data) the surgeon links the anatomical pictures with the knee or the hip CT scan data to the real life seen at the surgical field. Following careful analysis and assessment of the soft tissue is done. The robotic arm is utilised in preparing the bony surface to receive the implants. Trial implants are applied and after which replacement is done. Most patients are able to commence on therapy in the same day or the next day following surgery. This system has now been utilised in most patients for joint replacement presented for partial replacement selective for hip and knee replacement.
