OSTEOCHONDRAL INJURIES
Osteochondral injuries are becoming increasingly common in society. These are secondary to patients’ having a keen interest in sporting activities and also seen sometimes in weekend warrior syndromes. Patients when involving in sporting activities, it is very important to prime the soft tissue with appropriate stretches and strengthening exercises. When this is not done, patients can easily, incur twisting injuries, which can result in a myriad of soft tissue injuries, ranging from sprains, ligament tears to cartilage injuries.
In the knee, such injuries can present with swelling, locking, and instability. When patients are not improving in terms of their pain and swelling, beyond a period of 3-5 days, most times sprains are unlikely. In such instances, a further thorough clinical evaluation with X-rays and specialist assessment is important. In some cases, this may even require detailed imaging with MRI.
In a similar patient that was seen by Dr. Sathappan in the clinic, he presented with such symptoms of instability and locking. He is a 46-year-old gentleman who is an active soccer player. In such patients, degenerative cartilage injuries might be present and with a twisting injury in an unprimed soft tissue, he can easily sustain osteochondral injuries, such as this event happening while he was playing soccer.
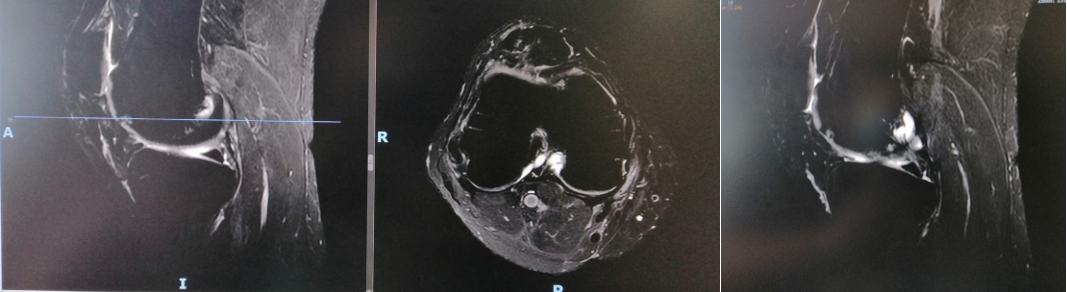
He tried the typical clinical management of RICE treatment (rest, ice, compression, elevation) for a protracted period of time. Despite such treatment, symptoms were persistent. Due to worsening pain and swelling, he presented to the clinic. Radiographs were unremarkable. Cartilage injuries usually are not evident in the X-rays, unless in the protracted period, sometimes, patients can have cystic changes in the subchondral region. Patient was then advised for MRI. MRI confirmed that this patient had an osteochondral injury involving the medial femoral condyle.
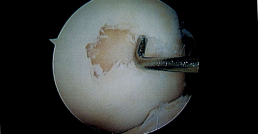
In view of his worsening symptoms, he was advised for surgical intervention. In the surgical procedure, he underwent a knee arthroscopy, which is a “keyhole” surgical procedure. At the time of surgery, as depicted in the clinical photographs, a distinct osteochondral lesion was noted. This is Grade IV lesion, where there is no more cartilage in that region due to the twisting injury which resulted in shaving off the cartilage at the time of impact.
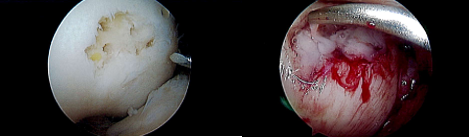
Following the initial surgical intervention of cleaning the knee, which in medical terms called arthroscopy, debridement, and synovectomy, the cartilage defect was then prepared. At the time of surgery, the preparation includes microfracture, which is to introduce fine holes into the subchondral bone. This allows bleeding to form and allows the fibrocartilage matrix to seal off the area. However, this fibrocartilage matrix is not strong enough and needs to be supported by a further chondral matrix or a scaffold. In this patient, option of CartiFill® was chosen. This is a very ideal scaffold for limited cartilage injuries, allowing to immediately cover and seal this area and at the same time provide structural support over a period of 4-6 weeks. When this is done, this allows us to assess the status of the cartilage, even during the scope because we are able to infiltrate with water and to assess the stability of the cartilage, unlike most other cartilage scaffolds. At the time of surgery, incidentally patient also had chondral injury in the patella. When such incidental injuries are seen, it is obligatory for the surgeon to try and alleviate the symptoms from presenting at a later point in time, when the physiotherapy intensifies. As such, the patient also had that addressed at the same time with the CartiFill options as clearly shown on the photographs.

Post-procedure, he was started on rehabilitation therapy. Rehabilitation therapy is a very crucial part of management of such osteochondral injuries. He was started on quadriceps and hamstrings strengthening exercises as well as progressive partial to full weight bearing exercises. This is important to prevent shearing of the cartilage matrix, which can cause recurring cartilage damage. Following this treatment, he was then started on intensive therapy and will be expected to return back to soccer activities at a period of approximately 4-6 months post-procedure.
Osteochondral injuries are increasingly common in patients in their 30s-60s mainly due to a very active lifestyle. If they are not treated effectively, these can lead to “kissing” lesions on the tibia as well as additional cartilage degeneration which can lead to osteoarthritis. This will then cause significant pain, locking and affect the patient’s quality of life. New technologies such as cartilage matrix and scaffold options that have been described facilitate in allowing the patients to return to optimal functional recovery at the shortest period of time.
Share this blog via:
- ← Deep Laceration from knife while cutting avocado
- SAVING A LIMB FROM AMPUTATION AFTER COMPLEX KNEE TRAUMA →