Running-related cartilage injury
This is a 51 year old gentleman who presented with worsening left knee pain. All his symptoms started after a running activity whereby he incurred in a severe pain following a twisting injury. Initially, he was been managed for knee sprains symptoms. He came to consult me because of persistent pain and swelling that had not resolved despite consultations with previous orthopaedic surgeons, Traditional Chinese medicine, physiotherapy. Due to worsening pain affecting walking, he was seen by me. As per the previous review by the clinician, X-rays were otherwise unremarkable except for osteoarthritis in the knee. His ambulation was atypical of simple degeneration. He was walking with a painful limp and medically term as antalgic gait. As part of the thorough clinical assessment, it was rather unusual why this 51 year old gentleman who has otherwise been running 3 to 5 times per week regularly should have difficulty.
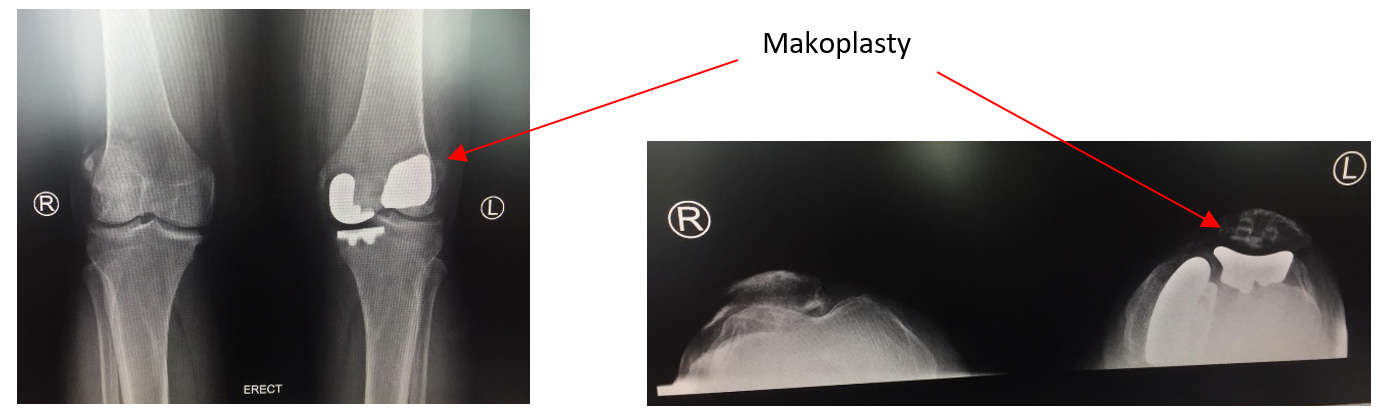
Based on my clinical assessment, I was rather concerned that he will have an osteochondral injury that will need further treatment. MRI was done which confirmed the clinical suspicion of osteochondral injury with marrow edema as seen in the attached MRI. There was also significant amount of effusion. The surgical options of knee arthroscopy, arthroplasty were discussed with the patient. His main concern was he wanted to continue running. Following a major procedure such as a total knee replacement, it would be difficult for patient to engage in high level of running activities since there is going to be replacement of the entire knee compartment. Thus, I offered him the options of arthroscopy versus partial replacement otherwise termed as Makoplasty. With arthroscopy and chondroplasty, the options are not long-term since the patient has got established knee osteoarthritis. Thus, I felt that this patient will be a much better candidate for partial replacement. During the clinical management, he requested for simple interventions such as viscosupplementations injection. These were attempted but were unsatisfactory due to the sizable injury in the medial compartment of the knee.
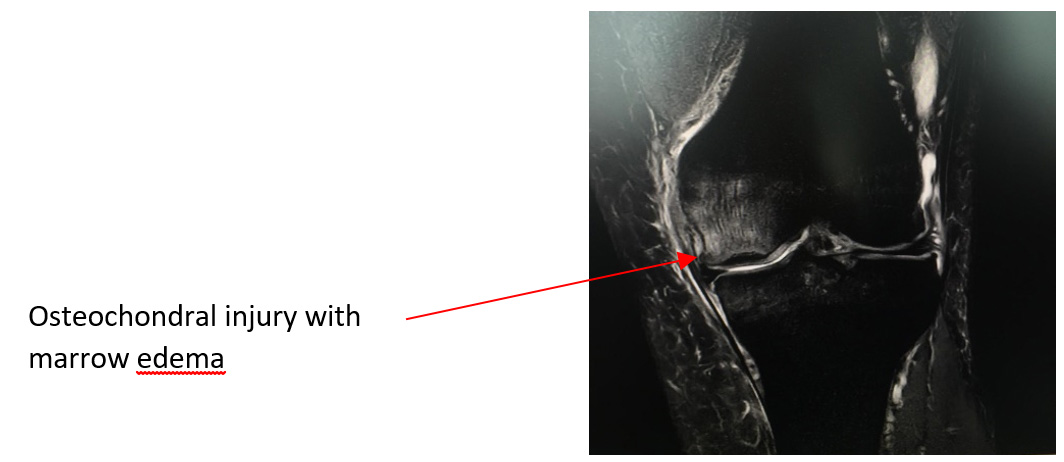
Subsequently, he also was seen by my sport therapist with limited improvement. His antalgic gait was worsening, and he opted to go for surgical procedure. At surgery, we found a very large osteochondral defect which was unsupported by the subchondral bone. In such settings, it is ideal to do a total knee replacement since it is a very highly predictable procedure. However, such a procedure involves sacrificing ligaments which may not give him the normal proprioceptive feel of the knee and thus makes his running difficult. During surgical assessment, after assessing the defect, I bone grafted the lesion giving substantial subchondral support for the replacement procedure. He underwent bicompartmental replacement which involves replacing both the medial compartment and the affected patellofemoral compartment. He recovered very well and completed 2 months of aggressive sports physiotherapy.

Following a good outcome, he has already returned back to jogging 6 months after his surgery and at last review has no major complains. His good outcome is typified by proper clinical assessment with good radiological support and physiotherapy to optimise the patient recovery to the fullest. Robotic surgery gives precision and enables the surgeon to accurately resurface the knee with minimal loss of natural ligament and cartilage tissue. Increasingly, we believe as clinicians that this has a big role to play in arthroplasty in patients as they drive towards to maintain a very active and aggressive lifestyle even after such surgeries.
Share this blog via:
- ← Patient presenting unusually with knee pain which is from the spine
- Benefits of robotic partial knee replacement (Makoplasty) →