Patient presenting unusually with knee pain which is from the spine
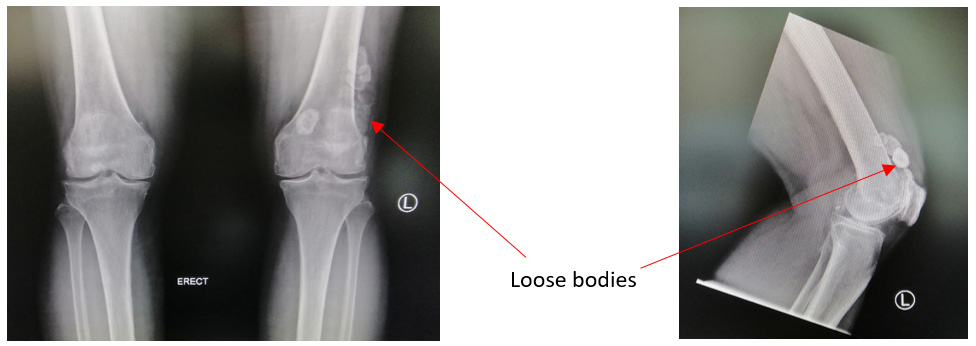
This 62 year old lady presented with worsening left knee pain. She was initially seen by an orthopaedic surgeon who have offered her knee arthroplasty based on her clinical diagnosis of osteoarthritis. She was told there were multiple loose bodies and that she will benefit from a knee replacement surgery. However, she was slightly concerned because the knee was associated with numbness and severe weakness in the left leg. The right leg also had severe osteoarthritis and she had no pain. Following her discussion with one of her friends she came to see me for a 2nd opinion.
As part of a thorough clinical assessment the physician has always got to take the full history and examination. This was done and it was noted that the patient’s symptoms of left knee pain were not localised to the knee. Let me explain. When there is mechanical pain from osteoarthritis patient’s were complained of pain, weakness, instability and swelling. The patient did not have any of these features and the pain seem to be inside the knee with no increase with palpation. When the patient is examined by the surgeon we always look for tenderness in the knee and physical examination suggestive of mechanical in nature. None of these were present in the patient. However, as part of the thorough assessment I also assess the patient’s spine condition. This is important because spine conditions can be associated with disc protrusion and such disc protrusion can press on the nerves around the knee. My physical examination was very suggestive of a spinal condition.
I reviewed her knee x-rays which are shown, do show a lot of loose bodies. However, it is very obvious that her left knee has far worst radiological symptoms with no pain. I convinced her that I was very concerned about a possible spine condition that has been missed by the previous clinician. She was referred for a MRI of the spine and it confirmed my clinical suspicion of a large disc that had extruded in the spine pressing on the L4 nerve root. This has resulted in severe radicular pain that was presenting with weakness and numbness. And this was localised to the left side associated with the background of foraminal stenosis.
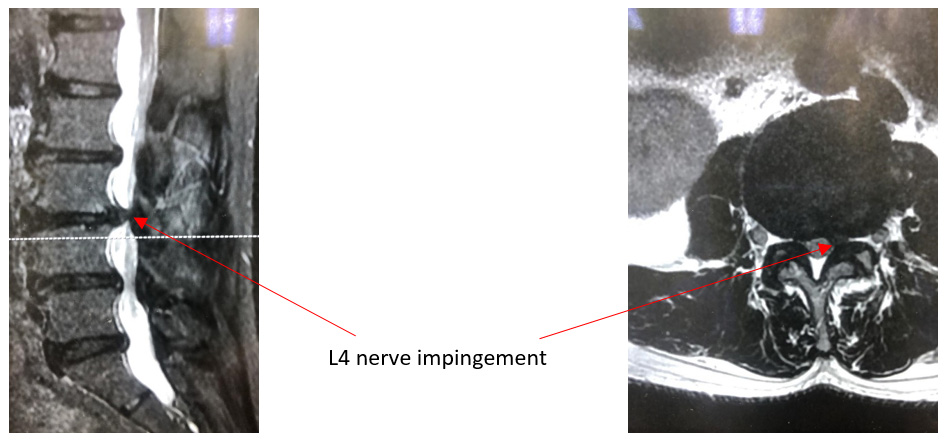
I discussed the interventional options. I told her she does not need knee replacement at this instant. However, it is probable that some of the mechanical pain may come back next time due to the numerous loose bodies in the left knee. The priority was however to treat the spine condition first. After a detailed discussion I advised her for spine decompression of the L3/L4 level where the nerve root was being compressed. Moreover, following the procedure at the same sitting I offered her the option of a knee arthroscopy and the removal of loose bodies. Following an informed consent, she underwent the procedure with a remarkable recovery. She is able to walk on the first day of the surgery and was discharged within 2days following the surgical procedure. After 1 month of regular physiotherapy in our clinic she has already returned to work with no limitation of all physical activities.
This clinical history emphasises that importance of not assuming that all pain at a particular site only arises from that particular anatomical region. It is very important to assess the patient holistically and evaluate whether the radiological investigation is compatible to the clinical findings. This will ensure that the clinical outcome of the patient is optimal.
Share this blog via: