SAVING A LIMB FROM AMPUTATION AFTER COMPLEX KNEE TRAUMA
This is a 40-year-old gentleman who was involved in a road traffic accident 2 years ago. He presented with acute open dislocation injury and had a pulseless leg with severe soft tissue injury to the knee. Following this injury, he had initial treatment with an external fixator to stabilise the lower limb as well as a four multiple compartment fasciotomy which is done to relieve the pressure in the four compartments of the leg. Moreover, he also had vascular reconstruction done to improve the vascularity of the leg. Following this injury, he had intravenous antibiotics to prevent infection.
In a knee dislocation injury, apart from the soft tissue such as the capsule, the supportive ligaments are usually torn. In this patient, he injured his posterolateral corner (PLC) and the medial collateral ligament (MCL) together with anterior cruciate ligament and the posterior cruciate ligament. The PLC and the MCL were all repaired following the surgery and he had wound coverage done by a split skin graft.

Unfortunately, in this patient, the vessels started to thrombose (form a clot) and the vascularity to the leg was compromised. When a healing wound, does not get regular blood supply, there remains a high risk of infection. In this patient, infection occurred and this compromised the viability of the leg. He was then advised for possible amputation of the leg.
He consulted Dr Sathappan for a second opinion initially via tele-consult and subsequently was transferred to his care. A thorough clinical history and examination was done and this confirmed the following clinical findings:
- Persistent absent pulses in particular dorsal pedis pulse (one of the 2 main arteries in the lower leg)
- Very weak posterior tibial pulse supplied by the collateral circulation (the other main artery)
- Myonecrosis (muscle death) involving anterolateral compartment
- Early septic arthritis (knee infection) due to the communicating positions of the wound to the knee joint
- Footdrop; a condition whereby the nerve to the leg was affected resulting in no active movement of the foot upwards
A thorough multi-disciplinary assessment and medical optimisation was done by Dr Sathappan and his team colleagues consisting of a reconstructive surgeon, vascular surgeon, infection disease specialist and intensivist.
The patient underwent 7 radical debridements and arthroscopic knee washouts. In the initial phases, debridements were often challenged by soft tissue dieback (tissues repeatedly “dieing” though initially appearing healthy). This indicates a situation whereby; the blood supply is so tenuous that the patient’s initial healing is always followed by some degree of soft tissue death and tissue loss. Eventually, optimal control of the infection was attained.
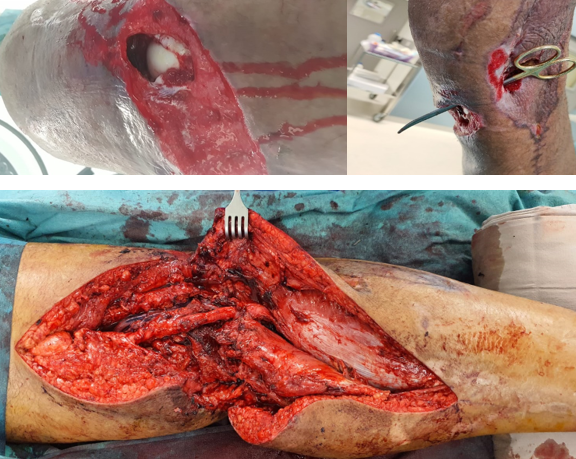
A detailed discussion on the subsequent management of coverage was discussed with the patient. Vascular status of the limb was assessed with an angiogram and showed that there was a 10cm cut off in the supply of the main circulation. He was then advised for wound coverage using a combination of soft tissue flaps and vascular reconstruction. He underwent the following surgical procedures at the same sitting consisting of:
- Wound debridement
- Arthroscopic knee washout
- Vascular reconstruction of artery and vein of the popliteal vessel
- A local muscle flap consisting of gastrocnemius muscle
- Nerve neurolysis of the sciatic nerve to free any scarring associated with the nerve in the injury
- Gracilis muscle flap to cover the wound
- A final latissimus dorsi muscle flap which is a free flap; consists of hooking up to a native blood supply to maintain the viability of the muscle since it is brought down from the shoulder region
- Vacuum-assisted dressing of the lower leg
- A bridging external fixator
Following this long, near 24-hour surgery, the patient was then managed in the ICU and then subsequently rehabilitated to the general ward.

Eventually, he had dynamization of the external fixator. This implies that the external fixator was progressively lightened, loosened, and patient was increasingly loaded with weight to improve the strength of the lower limb muscles.
With optimal team management as well as rehabilitation therapy, patient progressively improved. To facilitate coverage of the leg wound, a segment of the smaller bone called fibula was removed. Finally, the leg wound was covered with skin graft overlying the soft tissue site. With optimal rehabilitation, patient eventually had all his wounds covered, and regained improved knee range of motion. A brief timeline of what he underwent is listed below:
- Feb: 7 lower limb wound debridement with knee arthroscopic washout and vacuum dressing
- End Feb: Sciatic nerve neurolysis, Pedicled gastrocnemius muscle flap, Pedicled gracilis muscle flap, Free latissimus dorsi muscle flap, right lower limb wound debridement, Irrigation, Arthroscopic washout and External fixator of lower limb
- March: Wound debridement and vacuum dressing
- End March: Wound debridement and fibulectomy and right lower limb split skin graft of shin and wound closure
- April: Both lower wound debridement, dressing and external fixation adjustment
For this gentleman, he was about to lose his limb from the road traffic accident and due to the initial unsuccessful surgical procedure. However, multi-disciplinary approach with meticulous control of infection and multiple debridements together with increasing the vascularity by bringing in blood supply and covering this region with optimal tissue coverage allowed the patient to avoid leg amputation. It emphasises the need for a multi-disciplinary approach in achieving the goals of optimal patient recovery such as described in this case.
Knee dislocation injuries always remain a challenging injury to manage for the orthopaedic surgeons. It involves multiple soft tissue structures and especially the vascular segment, without which the viability of the leg will be vulnerable. Timely management of the soft tissue and the vascularity allowed in optimal recovery in this patient. He has already returned back to work and currently has no outstanding medical issues.




Share this blog via: